Discussion of case
The 28-yr-old female was having a malar rash, photosensitivity, dry eye and mouth, and fever (the only constitutional symptom) for the past three months. She was treated twice with antitubercular treatment - around two years back and a few days prior to the current referral. The probable diagnosis could be an autoimmune disease -SLE or related CTD, Still's disease, or vasculitis (remote possibility); infective condition - drug resistance-TB or other chronic viral infections including HIV or hepatitis.
Her positive ANA profile and presence of multiple autoantibodies suggest the diagnosis as SLE. The low TC, platelet, and complement levels also favor the diagnosis. The patient had persistent systemic symptoms for the past 2-3 years including intermittent fever. The history also revealed a previous episode of leukopenia and thrombocytopenia, but without malar rash. A careful evaluation of the history and the clinical investigation often help in making the diagnosis. However, a positive Widal test and a previous report of negative ANA suggested the possibility of other diagnoses.
The chances of over-diagnosing infectious diseases in primary care are relatively high and the common reason is high incidence. The unusual clinical presentations like low count, no localizing signs and symptoms, low-grade fever, high ESR, and low platelet count should raise suspicion of autoimmune diseases like SLE and other related diseases.
The EULAR/ACR Classification Criteria for Systemic Lupus Erythematosus is given below in table 1.
Table 1. EULAR/ACR Classification Criteria for Systemic Lupus Erythematosus1

Note -§ = additional criteria within the same domain will not be counted; * = in an assay with 90% specificity against relevant disease controls. Anti-β2GPI = anti–β2-glycoprotein I; anti-dsDNA = anti–double-stranded DNA
Fig 1: EULAR recommendations for SLE management2
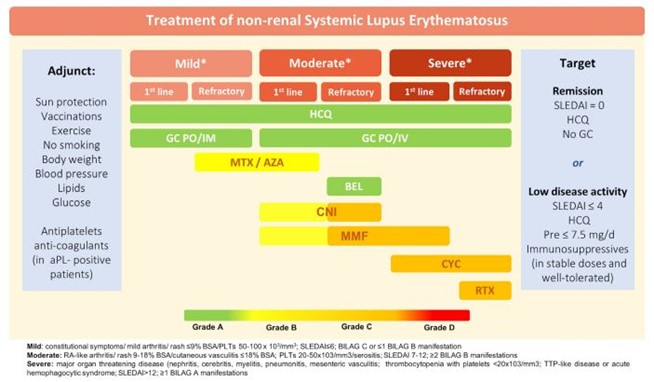
Note -aPL, antiphospholipid antibodies; AZA, azathioprine; BEL, belimumab; BILAG: British Isles Lupus Assessment Group disease activity index; CNIs, calcineurin inhibitors; CYC, cyclophosphamide; GC, glucocorticoids; HCQ, hydroxychloroquine; IM, intramuscular; MMF, mycophenolate mofetil; MTX, methotrexate; Pre, prednisone; PO, per os; RTX, rituximab; PLTs: Platelets; SLEDAI, Systemic Lupus Erythematosus Disease Activity Index.
The treatment of choice should be an adequate dose of NSAID to control the systemic features. Hydroxychloroquine and photoprotection measures including lifestyle changes should be recommended. If the patients fail to respond to the treatment, steroids and other immune modulators can be prescribed.
Learning points
- SLE needs a personalized approach.
- Steroid treatment is not necessary in all cases.
- ANA testing and other evidence are significant to confirm the diagnosis in patients suspected of SLE.
Reference
- Aringer M, Costenbader KH, Daikh DI, et al. 2019 EULAR/ACR Classification Criteria for Systemic Lupus Erythematosus. Arthritis Rheumatol. 2019;71(9):1400-1412. doi:10.1002/art.40930.
- Krieckaert CL, van Tubergen A, Gehin JE, et al. EULAR points to consider for therapeutic drug monitoring of biopharmaceuticals in inflammatory rheumatic and musculoskeletal diseases. Ann Rheum Dis. Published online May 11, 2022:annrheumdis-2022-222155. doi:10.1136/annrheumdis-2022-222155.