Discussion of case
55 years, female presented with back pain of inflammatory nature. She had both knee pain from the age of 40, with episodes of swelling, and inflammatory parameters being significantly elevated. The BMD indicated a significantly low score and no pathological fracture to date, The serum vitamin D levels were also normal. Radiological images of knee joints show normal knee joints, pelvis shows bilateral normal sacroiliac joints.
The clinical features suggestive of inflammatory backache, and lower limb arthritis, with minimal or no deformities, suggest a possibility of spondyloarthropathy. The other possibilities to be considered are degenerative arthropathy and infiltrative malignancy, especially multiple myeloma. However, all the probable causes of diagnosis one can consider are in Table 1.1
Table 1: Differential diagnoses
| Mechanical Low Back
or Leg Pain |
Non-mechanical Spinal
Conditions |
Visceral Disease |
| Lumbar strain or sprain
Degenerative processes of
disc and facets (usually
related to age)
Herniated disc
Spinal stenosis
Osteoporotic compression
fracture
Spondylolisthesis
Traumatic fractures
Congenital disease
Severe kyphosis
Severe scoliosis
Transitional vertebrae
Spondylolysis
Internal disc disruption or
discogenic back pain
Presumed instability |
Neoplasia
Multiple myeloma
Metastatic carcinoma
Lymphoma and leukemia
Spinal cord tumors
Retroperitoneal tumors
Primary vertebral tumors
Infection
Osteomyelitis
Septic discitis
Paraspinous abscess
Epidural abscess
Shingles
Inflammatory arthritis
Ankylosing spondylitis
Psoriatic spondylitis
Reiter syndrome
Inflammatory bowel disease (IBD)
Scheuermann disease
(osteochondrosis)
Paget's disease |
Pelvic organ involvement
Prostatitis
Endometriosis
Chronic pelvic inflammatory disease
Renal involvement
Nephrolithiasis
Pyelonephritis
Perinephric abscess
Aortic aneurysm
Gastrointestinal involvement
Pancreatitis
Cholecystitis
Penetrating ulcer |
The present case fulfills the ASAS classification criteria2 (figure 1 & 2) required for axial spondyloarthritis other than age and radiographic features. However, the possibility of spondyloarthropathy is relatively low for these female patients aged above 55 years. Radiographs of the knee and pelvis, and even that of the spine, do not suggest significant degenerative changes. Under the circumstances, one must consider the possibility of Infection including pelvic infection as well the malignancy like Multiple myeloma, as the inflammatory parameters are elevated. Evaluation of electrophoresis suggested an inflammatory pattern. Gynecological evaluation for pelvic infections and malignancy was found to be negative. The patient was HLA B 27 positive and anti-CCP negative.
ASAS classification criteria for axial and peripheral spondyloarthritis2
Fig 1 (A) ASAS classification criteria for axial spondyloarthritis.
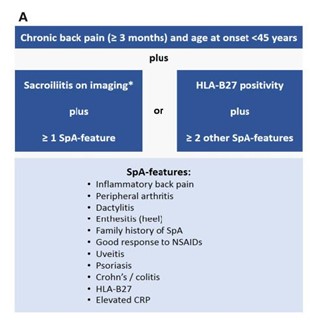
Fig 2 (B) ASAS classification criteria for peripheral spondyloarthritis.
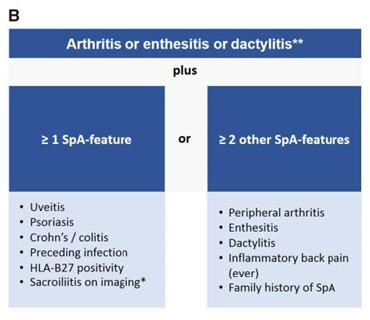
*Sacroiliitis on imaging refers to definite radiographic sacroiliitis according to the modified New York criteria or active sacroiliitis on MRI according to the ASAS definition. **Peripheral arthritis: usually predominantly lower limbs and/ or asymmetric arthritis; enthesitis: clinically assessed; dactylitis: clinically assessed. SpA: spondyloarthritis.
Spondyloarthropathy, though common in the younger age group, is adequately described in the literature. The clinical spectrum may vary, and age can be up to 70 years.3 The present patient fulfilled the ASAS criteria, in addition to being HLA B 27 positive and having elevated inflammatory parameters whereas the radiographic imaging indicates no damage to the knees and pelvic joints. Axial arthritis with no damage to the sacroiliac joints is considered non-radiographic axial spondyloarthropathy4.
Final Diagnosis
Non-axial Spondyloarthropathy HLA B 27 related.
Lesson to be learned
- Spondyloarthropathy can occur in the later age group
- Inflammatory parameters may be elevated in degenerative arthritis; it is usually not more than 2-3 folds.
- Suspicion and a careful workup will help in diagnosis.
References
- Jarvik, JG and Deyo RA. Diagnostic evaluation of low back pain with emphasis on imaging. Annals Int Med2002;137(7):586-597.
- Banegas Illescas ME, López Menéndez C, Rozas Rodríguez ML, Fernández Quintero RM. [New ASAS criteria for the diagnosis of spondyloarthritis: diagnosing sacroiliitis by magnetic resonance imaging]. Radiologia. 2014;56(1):7-15.
- Olivieri I, Padula A, Pierro A, Favaro L, Oranges GS, Ferri S. Late-onset undifferentiated seronegative spondyloarthropathy. J Rheumatol1995;22(5):899-903.
- Robinson PC, Sengupta R, Siebert S. Non-Radiographic Axial Spondyloarthritis (nr-axSpA): Advances in Classification, Imaging and Therapy. Rheumatol Ther. 2019;6(2):165-177. doi:10.1007/s40744-019-0146-6.